Clinical Research & Data, Patient Management, AMI Cardiogenic Shock
HFSA 2021: Managing AMI Cardiogenic Shock Using the National Cardiogenic Shock Initiative Study Protocol
Babar Basir, DO, FACC, FSCAI discusses acute myocardial infarction and cardiogenic shock (AMICS) and why he believes that the National Cardiogenic Shock Initiative (NCSI) protocol is the best way of treating AMICS in 2021. He gave this presentation virtually at the 2021 Heart Failure Society of America (HFSA) scientific meeting. Dr. Basir is the director of STEMI and acute mechanical circulatory support at Henry Ford Hospital in Detroit, MI.
Dr. Basir begins with recognizing the importance of shock phenotype—distinguishing between typical decompensated heart failure and AMI cardiogenic shock. He emphasizes that the decompensated heart failure patient has compensatory physiology not present in AMICS. “When you have compensatory physiology, you can actually challenge patients with inotropes and vasoactive medications to essentially restabilize their cardiac physiology,” he explains. “In an AMI population that comes with significant consequences… potentially worsening that infarct, worsening their long-term projection and their risk of having heart failure in the future as well.” The AMICS patient, Dr. Basir says, “needs much more robust and advanced hemodynamic support quicker.”
Dr. Basir discusses use of IABP, ECMO, and Impella® in these patients, stating that he believes that Impella is physiologically the best option for AMICS patients. He explains how Impella can rapidly decrease LVEDP and wall tension, improve coronary perfusion (if the coronaries are not completely occluded), improve cardiac power output (CPO), and decrease myocardial oxygen consumption. “These are all things that promote recovery and decrease infarct size. And so it’s really a great tool for us to be able to reverse shock very quickly.”
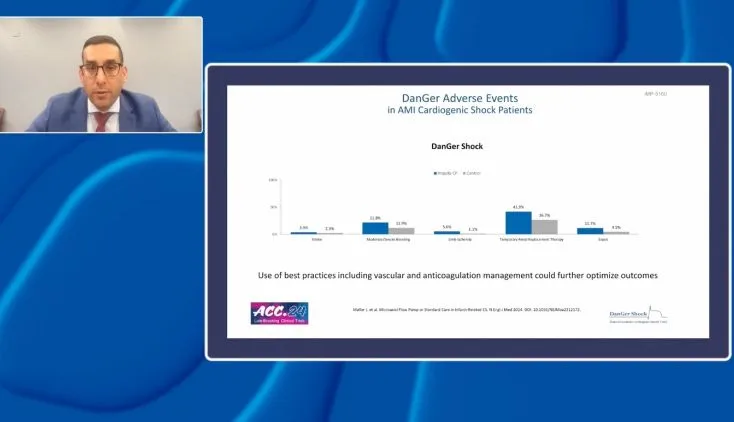
Dr. Basir then emphasizes the importance of using Impella in a systematic approach and sharing best practices to consistently achieve good outcomes. He explains that the National Cardiogenic Shock Initiative (NCSI) created a shock protocol studied in 80 centers across the country and now adopted in hundreds of centers throughout the world.
“One of the first important practices when using hemodynamic support in AMI is that we have to use the support early,” Dr. Basir explains. “As an interventionalist, it’s really important to me to emphasize that the support needs to go in quickly. In fact, it should ideally be put in before you go on to do the intervention.”
He also emphasizes the importance of invasive hemodynamics. “You cannot manage cardiogenic shock, particularly in an acute setting, without understanding what is actually hemodynamically happening with the patient.” Dr. Basir states that invasive hemodynamics is associated with survival, allowing for objective quantification of cardiogenic shock and greater utilization of advanced heart failure resources.
At the crux of the protocol, Dr. Basir explains, after the initial support device is in and the patient has been revascularized, it is important to “take a step back, look through their hemodynamics, and really spend some time here making the right decision for the patients.” It is at this critical point that he emphasizes getting the heart failure team involved.
The NCSI is the largest prospective North American AMICS study in the past 2 decades, recruiting the sickest cohort of patients in any major AMICS study. Outcomes from the study are encouraging, most notably 77% 30-day survival in patients with SCAI classes C and D shock. In his concluding remarks, Dr. Basir states, “We think that with more protocolization, more understanding of the importance of right ventricular support, escalation of support, that we can consistently get AMI shock survival rates greater than 80%.”
NPS-2334