Clinical Research & Data
CTO Impact on the Long-Term Prognosis of Ischemic Systolic Heart Failure
| Key Takeaways |
|---|
|
|
In 2016, the recorded prevalence of heart failure (HF) in the United States was 5.7 million, with an estimated 670,000 new diagnoses each year.1 The rates of post-discharge mortality and readmissions following treatment for HF have remained unchanged, despite the improvement in outcomes of ambulatory HF patients.2
Previous studies have shown that chronic total occlusion (CTO) of non-infarct-related arteries in hospitalized patients with acute coronary syndrome (ACS) correlates with higher incidences of in-hospital and long-term mortality compared with patients with no CTO. A registry-based study published in JACC: Cardiovascular Interventions evaluated the resulting long-term prognosis of ischemic systolic HF patients with CTO.3
A subgroup of consecutive non-selected patients (N=1157) who were hospitalized with heart failure symptoms and reduced left ventricular ejection fraction (LVEF) of ≤35% were included in this study for analysis. In 41.2% (n=278) of patients, at least 1 CTO of a coronary artery was observed. These patients also had a higher chance of suffering from a previous myocardial infarction (MI) and receiving coronary artery bypass grafting (CABG) compared with patients without CTO.
The CTO group in this study presented with a higher risk profile which included a history of MI, older age, diabetes prevalence, and greater percentage of multivessel coronary artery disease. Even after adjustment for baseline characteristics, a multivariate Cox analysis revealed that CTO independently increased 12-month mortality risk.
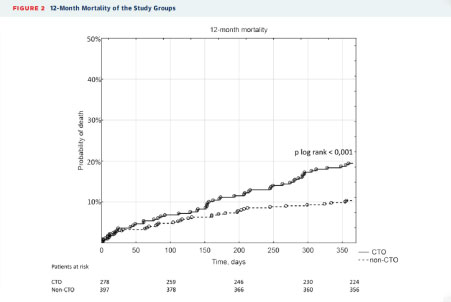
Figure 1. CTO vs Non-CTO Mortality at 12 Months3
At 12-month follow-up, 19.4% of the patients in the CTO group died, compared with 10.3% of the non-CTO group. This significant mortality difference was also documented at 2 years (26.6% vs 17.6% for CTO vs non-CTO, respectively). A multivariate analysis revealed that CTO independently increased 12-month mortality risk. In addition, twice as many patients in the CTO group died due to cardiovascular reasons (16.2% vs 8.3%).
The use of percutaneous coronary intervention (PCI) for CTO only occurred in 3.5% of patients, potentially contributing to the findings. Successful CTO PCI performed by experienced operators has previously been shown to improve LVEF and reduce left ventricular volume.4 Researchers suggest CTO PCI be more frequently considered to improve outcomes for these patients.
References
- Mozaffarian D, et al. (2016). Circulation, 133, e38-e360.
- Ambrosy AP, et al. (2014). J Am Coll Cardiol, 63(12), 1123-1133.
- Tajstra M, et al. (2016). JACC Cardiovasc Interv, 9(17), 1790-1797.
- Hoebers LP, et al. (2015). Int J Cardiol, 187, 90-96.
NPS-012-17