Are You Caring for Patients with Heart Disease?
Heart disease remains the nation’s leading cause of death1
About 655,000 Americans die from heart disease each year – an estimated 1 in every 4 deaths – with coronary artery disease (CAD) being the most common type of heart disease2. Epidemiological studies have Identified CAD as a major contributor to heart failure burden, with angiographic evidence of CAD being a significant marker for a worse heart failure prognosis, increasing mortality risk by 250%.2
- Estimated prevalence of CAD in patients with heart failure is 50-65%3
- CAD represents a potentially treatable or reversible cause of heart failure3
- Only 17.5% of patients with CAD who were hospitalized for new on-set heart failure were tested for ischemic coronary artery disease3
- Upfront ischemic testing can lead to lower resource utilization in terms of ED visits and rehospitalization for complications of CAD and heart failure3


Near Normal EF Patients Improved Heart Failure and Anginal Symptoms
Patients with near normal EF (>45%) experienced an 82% relative reduction in NYHA Class III and IV symptoms and a 97% relative reduction in CCS angina Class III and IV symptoms. High-risk PCI patients without depressed EF are likely to have more complex PCI and a high prevalence of comorbidities, according to data supporting the FDA's expanded indication for Impella use in high-risk PCI patients with or without depressed ejection fraction.4
A Growing Population Appropriate for PCI
Explore Protected PCI Resources
Patient Presentation Case Studies
Why is Protected PCI Important?
The use of the Impella heart pump during a PCI allows blood pressure to be maintained during the procedure, allowing the physician to perform a more complete and optimized procedure. Protected PCI with Impella heart pumps has been proven to improve quality of life for these patients and help them return home faster.2,3

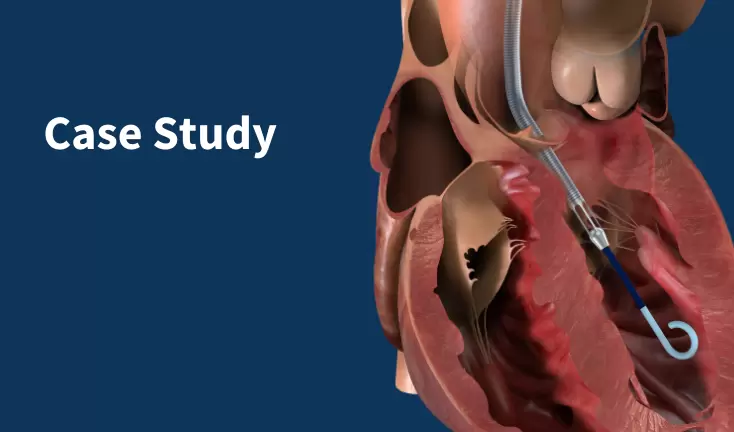
How Do Impella® Heart Pumps Work?
Impella, the world’s smallest heart pump, allows the heart to rest by protecting the patient hemodynamically during a high-risk procedure. Impella heart pumps provide direct left ventricular unloading by pulling blood from the left ventricle and expelling it into the aorta, increasing total cardiac output/arterial pressure and reducing myocardial oxygen consumption. For patients in right heart failure, the right-sided Impella heart pump delivers blood from the inferior vena cava to the pulmonary artery.
References
-
CDC: About Heart Disease
-
Velagaleti, R., et al., (2007). Cardio Clin, 25(4) 487-495.
-
Doshi D, et al., (2016). J Am Coll Cardiol, 68(5), 450-458.
- Wollmuth, J., Patel, M. et al. (2022). JSCAI, 100350. https://doi.org/10.1016/j.jscai.2022.100350
NPS-1478